CATEGORY 1 CME
Premiere Date: June 20, 2025
Expiration Date: December 20, 2026
This exercise provides CE credit for:
1. Physicians (CME)
2. Different
All different clinicians both will obtain a CME Attendance Certificates or could select any of the kinds of CE credit score being supplied.
ACTIVITY GOAL
To grasp the epidemiology of Parkinson illness signs.
LEARNING OBJECTIVES
1. Talk about the epidemiology of neuropsychiatric signs of Parkinson illness.
2. Describe the evaluation of neuropsychiatric signs of Parkinson illness.
3. Enumerate the evidence-based therapies for neuropsychiatric signs of Parkinson illness.
TARGET AUDIENCE
This accredited persevering with training (CE) exercise is meant for psychiatrists, psychologists, major care physicians, doctor assistants, nurse practitioners, and different well being care professionals who search to enhance their look after sufferers with psychological well being problems.
ACCREDITATION/CREDIT DESIGNATION/FINANCIAL SUPPORT
This exercise has been deliberate and applied in accordance with the accreditation necessities and insurance policies of the Accreditation Council for Persevering with Medical Schooling (ACCME) by the joint providership of Physicians’ Schooling Useful resource,® LLC and Psychiatric Instances®. Physicians’ Schooling Useful resource, LLC, is accredited by the ACCME to supply persevering with medical training for physicians.
Physicians’ Schooling Useful resource, LLC, designates this enduring materials for a most of 1.5 AMA PRA Class 1 Credit.™ Physicians ought to declare solely the credit score commensurate with the extent of their participation within the exercise.
This exercise is funded completely by Physicians’ Schooling Useful resource, LLC. No industrial assist was obtained.
OFF-LABEL DISCLOSURE/DISCLAIMER
This accredited CE exercise could or could not focus on investigational, unapproved, or off-label use of medicine. Contributors are suggested to seek the advice of prescribing data for any merchandise mentioned. The data offered on this accredited CE exercise is for persevering with medical training functions solely and isn’t meant to substitute for the impartial scientific judgment of a doctor relative to diagnostic or therapy choices for a particular affected person’s medical situation. The opinions expressed within the content material are solely these of the person college members and don’t mirror these of Physicians’ Schooling Useful resource, LLC.
FACULTY, STAFF, AND PLANNERS’ DISCLOSURES AND CONFLICT OF INTEREST MITIGATION
Not one of the workers of Physicians’ Schooling Useful resource, LLC, or Psychiatric Instances or the planners or the authors of this academic exercise have related monetary relationship(s) to reveal with ineligible firms whose major enterprise is producing, advertising, promoting, reselling, or distributing well being care merchandise utilized by or on sufferers.
For content-related questions, e mail us at PTEditor@mmhgroup.com; for questions in regards to the accreditation of this CME exercise or tips on how to declare credit score, please contact data@gotoper.com and embody “Impulse Management Issues, Psychosis, and Cognitive Impairment in Parkinson Illness” within the topic line.
HOW TO CLAIM CREDIT
Upon getting learn the article, please use the next URL to judge and request credit score: https://training.gotoper.com/exercise/ptcme25june. If you don’t have already got an account with Physicians’ Schooling Useful resource, LLC, you’ll be prompted to create one. You should have an account to judge and request credit score for this exercise.
Editor’s Notice: Please see the April CME article for extra data on despair, apathy, and nervousness in Parkinson illness.
Neuropsychiatric signs (NPS) are widespread amongst people with Parkinson illness (PD), with cross-sectional research indicating prevalence charges of 70% to 89%.1 Though widespread, these signs are sometimes underrecognized and never adequately handled, including to the incapacity attributable to the sickness.2 NPS which might be seen amongst people with PD embody despair, apathy, nervousness, impulse management problems (ICDs), psychosis, and cognitive impairment together with dementia. Despair, apathy, and nervousness have been coated in Half 1 of this CME exercise.
Psychosis
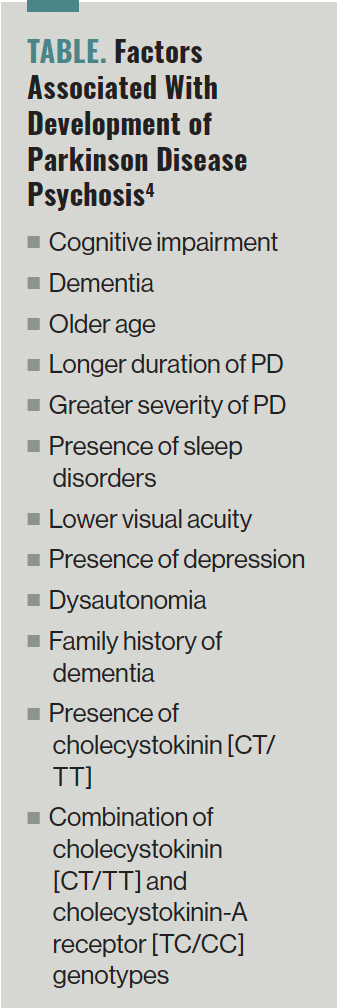
A meta-analysis by Chendo et al discovered that amongst people with PD, the pooled frequency of psychosis (hallucinations, delusions, and minor psychotic phenomena, together with sense of presence, passage hallucinations, and illusions) was 20.7%.3 In one other research, the investigators famous that visible hallucinations have been current in roughly 1 / 4 to a 3rd of people with PD and auditory hallucinations have been seen in about 20% of the people. Minor phenomena have been seen in roughly 17% to 72% of the people and delusions have been famous amongst 5% of the individuals with PD.4 Based on knowledge, additional components related to the event of PD psychosis (PDP) may be discovered within the Desk.4
TABLE. Elements Related With Growth of Parkinson Illness Psychosis4
Outcomes of 1 research confirmed that amongst people with PD and hallucinations at baseline (33%), the incidence of the hallucinations elevated to 44% at 18 months and 63% at 48 months (P <.0001).5 The investigators discovered that point was the one vital issue influencing the event of hallucinations over the 48-month interval. In lots of of those circumstances, hallucinations could develop into worse. One research discovered that hallucinations worsened in 95% of circumstances throughout a 3-year follow-up interval. A latest meta-analysis additionally discovered a big optimistic affiliation between psychosis and cognitive impairment (standardized imply distinction [SMD], 0.44), and psychosis and illness development (SMD, 0.46).6
Outcomes of one other meta-analysis confirmed that people with PDP have worse performing on all main cognitive domains compared with people with PD, however with out psychosis together with world cognition (Hedges g = —0.57), processing pace (Hedges g = —0.58), government capabilities (Hedges g = —0.56), episodic reminiscence (Hedges g = —0.58), and notion (Hedges g= —0.55) because the most certainly affected domains.7 One other meta-analysis discovered that people with PDP had decrease gray matter quantity (GMV) in parietal-temporo-occipital areas and the GMV loss in PDP was related to native gene expression of 5-HT1a (P = .012) and 5-HT2a receptors (P = .002) however not dopaminergic receptors.8
The consensus pointers developed by the Nationwide Institute of Neurological Issues and Stroke and the Nationwide Institute of Psychological Well being working group for the prognosis of PDP point out that for making a prognosis of PDP, a confirmed prognosis of PD with the onset of 1 or extra PDP-associated signs together with hallucinations, illusions, delusions, or false sense of presence with a length of no less than 1 month must be current.9 It is usually necessary to rule out secondary causes of psychosis together with medical, psychiatric, treatment results, and substance use problems. A prognosis of PDP may be made if the psychotic signs proceed regardless of elimination of different potential causes for psychosis.10 Half 1 of the Motion Dysfunction Society Unified Parkinson’s Illness Score Scale (UPDRS) and the improved Scale for the Evaluation of Optimistic Signs in PD which might be accomplished with the sufferers and their caregivers can help within the prognosis of PDP.
One meta-analysis discovered that cholinesterase inhibitors (CHIs) improved delusions (SMD, −0.14; P = .04) and hallucinations (SMD, —0.08; P = .01) amongst people with PD.11 Though there have been no vital variations famous among the many varied CHIs, rivastigmine confirmed the biggest impact measurement for each delusions (SMD, —0.11; P = .03) and hallucinations (SMD, —0.10; P = .01). The investigators additionally discovered a big impact measurement for CHIs on the overall neuropsychiatric rating (SMD, —0.18; P = .002). Additionally they famous a big interplay between the therapy impact and the baseline neuropsychiatric whole rating (P = .02) compared with placebo, indicating that a rise in baseline neuropsychiatric rating elevated the impact measurement in favor of treatment therapy. A major interplay between therapy consequence of whole neuropsychiatric rating and baseline Mini Psychological State Examination (MMSE) rating was famous (P = .008), indicating {that a} lower in baseline MMSE rating elevated the impact measurement in favor of treatment therapy compared with placebo.
In one other community meta-analysis, Yunusa et al discovered that on the Scientific International Impression Scale for Severity, pimavanserin (SMD, —4.81), clozapine (SMD, —4.25), and quetiapine (SMD, —1.15) considerably improved severity of psychotic signs compared with placebo.12 On the Scale for Evaluation of Optimistic Signs for Parkinson Illness, pimavanserin (OR, 1.16) improved psychotic signs compared with placebo. On the UPDRS, clozapine (SMD, −0.69), pimavanserin (SMD, —0.01), and quetiapine (SMD, 0.00) didn’t impair motor functioning. Quetiapine (SMD, 0.60) impaired cognition (MMSE scores) compared with placebo. Outcomes of this research discovered that pimavanserin and clozapine have been most efficacious and secure with pimavanserin having the best likelihood of being efficacious when used amongst people with PDP. Pimavanserin is FDA accredited for the therapy of PDP.
In a second community meta-analysis, Srisurapanont et al discovered that clozapine (SMD, —1.31) and pimavanserin (SMD, —0.30) have been superior to the placebo in treating psychotic signs amongst people with PD, whereas quetiapine (SMD, 0.47) was discovered to be inferior to placebo.13 Clozapine was ranked first in lowering psychotic signs (P-score = 1.00), adopted by pimavanserin (P-score = 0.73). Clozapine was ranked first (P-score = 0.81) in stopping the worsening of irregular actions. The authors concluded that clozapine emerged because the treatment with the best efficacy (massive therapy impact) and exhibited minimal motor hostile results, had excessive acceptability and average total tolerability. Pimavanserin was ranked second when it comes to efficacy (small-to-moderate therapy impact) and was related to average motor hostile results, total tolerability, and acceptability.
One meta-analysis that evaluated knowledge from 5 research discovered that electroconvulsive remedy (ECT) was efficient in treating psychotic signs amongst people with PD (SMD, 1.64, P <.001).14 Outcomes of this research additionally confirmed that cognition improved after ECT amongst these people (SMD, 0.21; P = .002).
Out there proof from these research signifies that pimavanserin and clozapine are first-line drugs to deal with psychotic signs amongst people with PD. Quetiapine may be thought-about as a second-line treatment to deal with signs of PDP. CHIs, particularly rivastigmine, can also be helpful in therapy of PDP. ECT can be utilized for the therapy of psychotic signs that aren’t amenable to therapy with pimavanserin, clozapine, and/or quetiapine.
ICDs
ICDs are characterised by an incapacity to withstand an inappropriate drive, leading to repetitive behaviors that may result in dangerous penalties to the person.15 The commonest ICDs embody pathological playing, compulsive sexual habits, compulsive consuming, and compulsive purchasing. ICDs are seen in roughly 18.5% of people with PD.16 Impulsive-compulsive behaviors (ICBs) consult with repetitive, extreme, and compulsive behaviors which might be pushed by some sturdy want and are sometimes tough to regulate. ICBs are seen in roughly 14.64% of people with PD.17
Out there proof signifies that the ICD worsens high quality of life, actions of every day dwelling, and emotional well-being (P <.004) amongst people with PD.18 One meta-analysis discovered that compared with people who’ve PD and no ICD, people with PD and ICD had worse abstraction means/idea formation (Hedges g = —0.40), set shifting (Hedges g = —0.59 and —0.46), visuospatial/constructional means (Hedges g = —0.42), and decision-making (Hedges g = 0.54).19
One meta-analysis that included knowledge from 15 research discovered that threat components for people with PD growing ICD have been youthful age (SMD, —0.39, P <.01), male intercourse (OR, 1.64; P <.01), smoking behavior (OR, 2.28; P = .02), dopamine receptor agonist (DA) use (OR, 3.41; P <.01), DA equal every day dose (SMD, 0.42; P = .003), levodopa equal every day dose (whole LEDD; SMD, 0.32; P <.01), and amantadine use (OR, 2.26; P <.01).20
ICBs have been famous to be extra widespread amongst Caucasians (17.9%) than amongst Asians (12.4%) with PD.17 Threat components for ICBs amongst people with PD are youthful age (P <.0001), male intercourse (OR, 1.64; P = .001), longer course of PD (P = .005), increased despair scores (Hamilton Despair Score Scale, P = .007), extra levodopa dosage (P = .02), DA use (P <.00001), increased common dose (levodopa, P = .0003; DA, P <.00001), in addition to extra amantadine use (P = .0004). One meta-analysis additionally discovered that fast eye motion habits dysfunction was related to a greater than 2-fold larger threat of growing ICBs (OR, 2.12; P <.01).21
A meta-analysis discovered that there have been no vital adjustments in any cortical or subcortical areas amongst people with PD and ICD.22 Nonetheless, there was elevated exercise famous within the ventral striatum and orbitofrontal cortex and decreased exercise in anterior cingulate cortex (ACC) amongst these people. Moreover, clusters of hyperactivation in ventral striatum and of hypoactivation in ACC have been additionally famous within the meta-analysis. These findings point out strongly that ICD in PD is said to a dysfunction of limbic divisions of the striatum and of the prefrontal cortex. One meta-analysis discovered that there was no vital impairment recognized in reward processing in sufferers with PD and ICD compared with sufferers with PD and with out ICD (SMD, −0.02; 95% CI, —0.43-0.39).
A prognosis of ICD is made by way of a scientific interview with the person with PD and their caregivers.23 Questionnaire for ICDs in PD and Questionnaire for ICDs in PD Score Scale are validated scales with a sensitivity of 96% and 94%, respectively, in figuring out ICDs amongst people with PD.24
Though there are not any meta-analyses which have evaluated the therapies for ICDs amongst people with PD, therapy suggestions embody lowering and even withdrawing DAs as a first-line technique.25 Using intrajejunal levodopa that gives steady drug supply to the physique or utilizing amantadine, which acts as a dopaminergic and glutamatergic modulator, could profit some people with ICD with out aggravating motor capabilities. Restricted knowledge additionally point out some profit from valproate, zonisamide, naloxone, apomorphine, and bromocriptine amongst people with ICD. Clozapine could also be helpful for the therapy of refractory ICDs amongst people with PD.26 Though the information are restricted, a number of research additionally advocate subthalamic nucleus deep mind stimulation as a therapy for ICDs.25 Low-frequency repetitive transcranial magnetic stimulation (rTMS) over the dorsolateral prefrontal cortex has additionally been famous to be helpful amongst people with PD and ICBs.27 One randomized managed trial that in contrast as much as 12 classes of a cognitive habits remedy (CBT)-based intervention to a ready listing management situation with normal medical care indicated that ICBs improved considerably within the therapy group compared with controls (P = .03).28
These research point out that discontinuation of DAs and using CBT could also be first choices for treating ICDs/ICBs amongst people with PD. Medicines equivalent to clozapine and coverings equivalent to rTMS could also be helpful amongst refractory circumstances of ICDs/ICBs.
Cognitive Impairment
Amongst people with PD, cognitive impairment is among the main nonmotor signs.29 Cognitive impairment presents insidiously amongst people with PD and consists of impairments in planning, working reminiscence, government dysfunction, consideration, semantic verbal fluency, and visible spatial means. People with PD could subsequently develop delicate cognitive impairment (MCI), which can progress to dementia. Outcomes of a meta-analysis discovered that postural-instability-gait dysfunction (RR, 3.76), hallucinations (RR, 3.09), orthostatic hypotension (RR, 2.98), cerebrovascular illness (RR, 1.52), diabetes (RR, 1.47), weight problems (RR, 1.38), cardiac illness (RR, 1.35), and alcohol consumption (RR, 1.32) improve the danger for cognitive impairment amongst people with PD.30
One meta-analysis discovered that the pooled prevalence of MCI was 40%, with the next frequency for the a number of area subtype (31%) of MCI to be seen amongst people with PD.31 Threat components for growing MCI in PD have been older age (Hedges g = 0.36), male intercourse (Hedges g = 0.10), decrease ranges of training (Hedges g = —0.29), an extended illness length (Hedges g = 0.18), use of upper LEDD (Hedges g = 0.25), increased Hoehn and Yahr stage (Hedges g = 0.33), increased UPDRS motor scores (Hedges g = 0.40), postural instability/gait issue motor subtype vs tremor dominant subtype (46% vs 35%; P <.001), despair (Hedges g = 0.29), apathy (Hedges g = 0.41), and a poorer high quality of life (Hedges g = 0.18). One meta-analysis that included knowledge from 39 research discovered that inside 3 years, 25% of people with PD and regular cognition transformed to PD-MCI, and a pair of% transformed to dementia.32 Of these with PD-MCI, 20% transformed to dementia, whereas 28% reverted to a state of regular cognitive operate. The investigators famous that the conversion charges to MCI and dementia have been increased and reversion charges have been decrease when the follow-up was equal to or longer than 3 years. A meta-analysis revealed that amongst all of the cognitive domains (Hedges g = 0.47), measures of government functioning (Hedges g = 0.70) predicted the conversion of people with PD-MCI to PD dementia (PDD).33
One meta-analysis discovered that the worldwide pooled dementia frequency amongst people with PD was 26.3%.34 The pooled frequency of dementia was larger amongst people aged 75 years or older (43.4%), lower than or equal to 4 years of training (29.2%), 15 years or longer of PD length (40.9%), and larger than 3 on the Hoehn and Yahr stage (45.9%). A latest meta-analysis discovered that the pooled incidence charge of PDD was 4.45 per 100 person-years in danger, equating to a 4.5% annual threat of dementia in a PD-prevalent inhabitants.35 The relative threat of PDD was estimated to be 3.25 instances larger than in wholesome controls. One other meta-analysis discovered that the event of PDD was positively related to older age (OR, 1.07), male intercourse (OR, 1.33), increased UPDRS half III scores (RR, 1.04), presence of hallucinations (OR, 2.47), REM sleep habits dysfunction (OR, 8.38), smoking (ever vs by no means: RR, 1.93), and hypertension (OR, 1.57).36 An inverse affiliation was discovered between training (RR, 0.94) and the event of PDD. One meta-analysis that included knowledge from 17 research analyzed the affect of the APOE gene on PDD onset from 3 features: 5 genotypes vs ε3/3, ε2+/ε4+ vs ε3/3, and ε4+ vs ε4−, and located that the danger components for PDD embody the genotypes ε3/4 (OR, 1.47) and ε4/4 (OR, 2.93; 95% CI, 1.20-7.14).37 The danger of PDD was 1.61 instances larger in ε4+ people compared with ε3/3 people (OR, 1.61; P = .0003). Amongst people with PD, the dementia threat of these with ε4+ was 1.72 instances larger than that of these with ε4− (OR, 1.72; P <.00001).
You will need to usually consider cognitive functioning amongst people with PD given the prevalence of cognitive impairment amongst them.38 The presence of a cognitive dysfunction may be recognized utilizing validated screening instruments or by a proper neuropsychological evaluation. It is usually necessary to finish a full medical examination together with laboratory workup to rule out the potential medical causes for cognitive impairment. The Worldwide Parkinson and Motion Dysfunction Society recommends 3 score scales based mostly on their clinimetric properties to measure world cognitive efficiency amongst people with PD.39 These 3 scales are the Montreal Cognitive Evaluation (MoCA), the Mattis Dementia Score Scale Second Version, and the Parkinson’s Illness-Cognitive Score Scale. The MoCA is probably the most ceaselessly used cognitive screening device in scientific apply and analysis research amongst people with PD. Out there proof signifies that normed neuropsychological exams throughout a number of cognitive domains can persistently detect cognitive deficits amongst people with PD, however relative PD efficiency is considerably affected by the inclusion and the kind of wholesome controls vs using revealed norms solely.40 It is crucial that the number of exams be executed based mostly on the presence of satisfactory native inhabitants norms.
At present, there are not any FDA-approved nonpharmacologic or pharmacologic therapies for MCI amongst people with PD.41 Preliminary proof signifies that cognitive coaching and bodily train could have short-term advantages on government functioning amongst people with PD.38 Multidomain computer-based cognitive coaching at a frequency of two or 3 instances per week over 3 to 12 weeks could enhance government capabilities, reminiscence, processing pace, and a spotlight.38 Cardio train, resistance train, and mixed bodily and cognitive coaching could present short-term advantages on world cognition, processing pace, sustained consideration, psychological flexibility, and reminiscence amongst people with PD.38
Simply oral rivastigmine is FDA accredited for the therapy of mild-to-moderate PDD.38 One meta-analysis discovered that amongst people with PDD, compared with placebo, CHI therapy improved scores on the Alzheimer Illness Cooperative Research—Scientific International Impression of Change (P <.0001).42 For cognitive operate, a pooled estimate of the impact of CHIs on measures of cognitive operate confirmed therapeutic profit (SMD, —0.34; P <.00001). There was additionally a optimistic impact of CHIs on the MMSE (weighted imply distinction [WMD], 1.09; P = .0008). For actions of every day dwelling, mixed knowledge for the Alzheimer Illness Cooperative Research—Scientific International Impression of Change and the UPDRS score scales favored therapy with CHIs (SMD, —0.20; P = .03). For security and tolerability, these taking a CHI have been extra more likely to expertise an hostile occasion (OR, 1.64; P = .0003) and to drop out (OR, 1.94; P = .0006). Hostile occasions have been extra widespread amongst these taking rivastigmine (OR, 2.28; P <.0001) however not these taking donepezil (OR, 1.24; P = .25). Tremors (OR, 2.71; P = .002), however not falls (P = .39), have been extra widespread within the therapy group however it didn’t have a big affect on the UPDRS (whole and motor scores, P = .71). Fewer deaths occurred within the therapy group than within the placebo group (OR, 0.28; P = .03).
One other meta-analysis that included knowledge from 10 trials discovered that CHIs and memantine produced small world results on clinicians’ world impression of change (WMD, —0.40 to WMD, —0.65).43 Nonetheless, simply CHIs and never memantine improved cognition on the MMSE (WMD, 1.04 to 2.57 vs 0.45). Rivastigmine confirmed an elevated threat of hostile occasions compared with placebo (RR, 1.19), though these have been delicate or average, and the danger disappeared on severe hostile occasions.
A 3rd meta-analysis research that solely included individuals with PD discovered that CHIs considerably slowed MMSE decline (MD, —1.123; P = .0010) with none impact on threat of falls (OR, 1.134; P = .681).44 The charges of tremors (OR, 2.805; P = .001) and hostile drug reactions (OR, 1.86; P <.0001) have been considerably elevated in sufferers receiving CHIs in contrast with placebo. When put next with placebo, the Alzheimer’s Illness Evaluation Scale–Cognitive Subscale (SMD, —0.266; P <.0001), world evaluation (SMD, —0.287, P <.0001), and behavioral disturbances (SMD, —0.152; P = .025) improved within the CHI group with none impact on incapacity (SMD, —0.134; P = .053). There have been no vital variations between the two teams on the UPDRS half III scores (SMD, 0.054; P = .805). The demise charge was decreased within the CHI group compared with placebo (OR, 0.295; P = .017).
In a fourth meta-analysis, investigators decided that people with PDD who obtained donepezil (SMD, 0.51; P <.00001) or rivastigmine (SMD, 0.45; P <.00001) discovered advantages on world cognitive scores compared with placebo.45 On the Scientific International Impressions of Change scale, vital enhancements have been famous in individuals who obtained rivastigmine compared with placebo (RR, 1.37). Rivastigmine in PDD offered a big profit for tremor compared with placebo (MD, —2.32; P <.00001). Simply people handled with rivastigmine skilled considerably extra hostile occasions compared with placebo (RR, 1.18; P = .0001).
These research point out that nonpharmacologic therapies equivalent to cognitive coaching and bodily train could have short-term advantages on cognition amongst people with PD. Oral rivastigmine is the one FDA-approved agent for the therapy of mild-to-moderate PDD, though different CHIs could also be of profit amongst people with PDD.
Concluding Ideas
NPS are seen generally amongst people with PD. These embody despair, apathy, nervousness, ICDs, psychosis, and cognitive impairment together with dementia. Regardless of being widespread, the NPS are poorly recognized and poorly handled amongst people with PD. NPS worsen morbidity and high quality of life amongst people with PD. Out there proof signifies advantages for nonpharmacologic therapies, pharmacotherapeutic brokers, and for mind stimulation strategies amongst people with PD who’ve NPS. Earlier identification and applicable therapy of people with PD who’ve NPS will considerably enhance the lives of those people and people of their caregivers.
Dr Tampi is professor and chairman of the Division of Psychiatry at Creighton College Faculty of Drugs and Catholic Well being Initiatives Well being Behavioral Well being Companies in Omaha, Nebraska. He’s additionally an adjunct professor of psychiatry at Yale Faculty of Drugs, New Haven, Connecticut. Ms Snyder is a medical scholar at Creighton College Faculty of Drugs, Omaha, NE.
References
1. Dlay JK, Duncan GW, Khoo TK, et al. Development of neuropsychiatric signs over time in an incident Parkinson’s illness cohort (ICICLE-PD). Mind Sci. 2020;10(2):78.
2. Jones S, Torsney KM, Scourfield L, et al. Neuropsychiatric signs in Parkinson’s illness: aetiology, prognosis and therapy. BJPsych Advances. 2020;26(6):333-342.
3. Chendo I, Silva C, Duarte GS, et al. Frequency and traits of psychosis in Parkinson’s illness: a scientific evaluation and meta-analysis. J Parkinsons Dis. 2022;12(1):85-94.
4. Fénelon G, Alves G. Epidemiology of psychosis in Parkinson’s illness. J Neurol Sci. 2010;289(1-2):12-17.
5. Goetz CG, Leurgans S, Pappert EJ, et al. Potential longitudinal evaluation of hallucinations in Parkinson’s illness. Neurology. 2001;57(11):2078-2082.
6. Burchill E, Watson CJ, Fanshawe JB, et al. The affect of psychiatric comorbidity on Parkinson’s illness outcomes: a scientific evaluation and meta-analysis. Lancet Reg Well being Eur. 2024;39:100870.
7. Pisani S, Gosse L, Wieretilo R, et al. Cognitive and government impairments in Parkinson’s illness psychosis: a Bayesian meta-analysis. J Neurol Neurosurg Psychiatry. 2024;95(3):277-287.
8. Pisani S, Gunasekera B, Lu Y, et al. Gray matter quantity loss in Parkinson’s illness psychosis and its relationship with serotonergic gene expression: a meta-analysis. Neurosci Biobehav Rev. 2023;147:105081.
9. Ravina B, Marder Ok, Fernandez HH, et al. Diagnostic standards for psychosis in Parkinson’s illness: report of an NINDS, NIMH work group. Mov Disord. 2007;22(8):1061-1068.
10. Pagan FL, Schulz PE, Torres-Yaghi Y, Pontone GM. On the optimum prognosis and the evolving position of pimavanserin in Parkinson’s illness psychosis. CNS Medicine. 2024;38(5):333-347.
11. d’Angremont E, Begemann MJH, van Laar T, Sommer IEC. Cholinesterase inhibitors for therapy of psychotic signs in Alzheimer illness and Parkinson illness: a meta-analysis. JAMA Neurol. 2023;80(8):813-823.
12. Yunusa I, Rashid N, Seyedin R, et al. Comparative efficacy, security, and acceptability of pimavanserin and different atypical antipsychotics for Parkinson’s illness psychosis: systematic evaluation and community meta-analysis. J Geriatr Psychiatry Neurol. 2023;36(5):417-432.
13. Srisurapanont M, Suradom C, Suttajit S, et al. Second-generation antipsychotics for Parkinson’s illness psychosis: a scientific evaluation and community meta-analysis. Gen Hosp Psychiatry. 2024;87:124-133.
14. Takamiya A, Seki M, Kudo S, et al. Electroconvulsive remedy for Parkinson’s illness: a scientific evaluation and meta-analysis. Mov Disord. 2021;36(1):50-58.
15. Bugalho P, Oliveira-Maia AJ. Impulse management problems in Parkinson’s illness: crossroads between neurology, psychiatry and neuroscience. Behav Neurol. 2013;27(4):547-557.
16. Macías-García P, Rashid-López R, Cruz-Gómez ÁJ, et al. Neuropsychiatric signs in clinically outlined Parkinson’s illness: an up to date evaluation of literature. Behav Neurol. 2022;2022:1213393.
17. Cao L, Xu T, Zhao G, et al. Threat components of impulsive-compulsive behaviors in PD sufferers: a meta-analysis. J Neurol. 2022;269(3):1298-1315.
18. Phu AL, Xu Z, Brakoulias V, et al. Impact of impulse management problems on incapacity and high quality of life in Parkinson’s illness sufferers. J Clin Neurosci. 2014;21(1):63-66.
19. Santangelo G, Raimo S, Barone P. The connection between impulse management problems and cognitive dysfunctions in Parkinson’s illness: a meta-analysis. Neurosci Biobehav Rev. 2017;77:129-147.
20. Liu B, Luo W, Mo Y, et al. Meta-analysis of associated components of impulse management problems in sufferers with Parkinson’s illness. Neurosci Lett. 2019;707:134313.
21. Lu HT, Shen QY, Zhao QZ, et al. Affiliation between REM sleep habits dysfunction and impulsive-compulsive behaviors in Parkinson’s illness: a scientific evaluation and meta-analysis of observational research. J Neurol. 2020;267(2):331-340.
22. Santangelo G, Raimo S, Cropano M, et al. Neural bases of impulse management problems in Parkinson’s illness: a scientific evaluation and an ALE meta-analysis. Neurosci Biobehav Rev. 2019;107:672-685.
23. Weintraub D, Claassen DO. Impulse management and associated problems in Parkinson’s illness. Int Rev Neurobiol. 2017;133:679-717.
24. Weintraub D, Hoops S, Shea JA, et al. Validation of the questionnaire for impulsive-compulsive problems in Parkinson’s illness. Mov Disord. 2009;24(10):1461-1467.
25. Zhang JF, Wang XX, Feng Y, et al. Impulse management problems in Parkinson’s illness: epidemiology, pathogenesis and therapeutic methods. Entrance Psychiatry. 2021;12:635494.
26. Bonfils NA, Benyamina A, Aubin HJ, Luquiens A. Clozapine use for refractory impulse management problems in Parkinson’s illness: a case report. Psychopharmacology (Berl). 2015;232(19):3677-3679.
27. Nardone R, De Blasi P, Höller Y, et al. Repetitive transcranial magnetic stimulation transiently reduces punding in Parkinson’s illness: a preliminary research. J Neural Transm (Vienna). 2014;121(3):267-274.
28. Okai D, Askey-Jones S, Samuel M, et al. Trial of CBT for impulse management behaviors affecting Parkinson sufferers and their caregivers. Neurology. 2013;80(9):792-799.
29. Fang C, Lv L, Mao S, et al. Cognition deficits in Parkinson’s illness: mechanisms and therapy. Parkinsons Dis. 2020;2020:2076942.
30. Guo Y, Xu W, Liu FT, et al. Modifiable threat components for cognitive impairment in Parkinson’s illness: a scientific evaluation and meta-analysis of potential cohort research. Mov Disord. 2019;34(6):876-883.
31. Baiano C, Barone P, Trojano L, Santangelo G. Prevalence and scientific features of delicate cognitive impairment in Parkinson’s illness: a meta-analysis. Mov Disord. 2020;35(1):45-54.
32. Saredakis D, Collins-Praino LE, Gutteridge DS, et al. Conversion to MCI and dementia in Parkinson’s illness: a scientific evaluation and meta-analysis. Parkinsonism Relat Disord. 2019;65:20-31.
33. Wallace ER, Segerstrom SC, van Horne CG, et al. Meta-analysis of cognition in Parkinson’s illness delicate cognitive impairment and dementia development. Neuropsychol Rev. 2022;32(1):149-160.
34. Severiano E Sousa C, Alarcão J, Pavão Martins I, Ferreira JJ. Frequency of dementia in Parkinson’s illness: a scientific evaluation and meta-analysis. J Neurol Sci. 2022;432:120077.
35. Gibson LL, Weintraub D, Lemmen R, et al. Threat of dementia in Parkinson’s illness: a scientific evaluation and meta-analysis. Mov Disord. 2024;39(10):1697-1709.
36. Xu Y, Yang J, Shang H. Meta-analysis of threat components for Parkinson’s illness dementia. Transl Neurodegener. 2016;5:11.
37. Pang S, Li J, Zhang Y, Chen J. Meta-analysis of the connection between the APOE gene and the onset of Parkinson’s illness dementia. Parkinsons Dis. 2018;2018:9497147.
38. Aarsland D, Batzu L, Halliday GM, et al. Parkinson disease-associated cognitive impairment. Nat Rev Dis Primers. 2021;7(1):47.
39. Skorvanek M, Goldman JG, Jahanshahi M, et al; members of the MDS Score Scales Overview Committee. International scales for cognitive screening in Parkinson’s illness: critique and suggestions. Mov Disord. 2018;33(2):208-218.
40. Hoogland J, van Wanrooij LL, Boel JA, et al; IPMDS Research Group. Detecting delicate cognitive deficits in Parkinson’s illness: comparability of neuropsychological exams. Mov Disord. 2018;33(11):1750-1759.
41. Solar C, Armstrong MJ. Remedy of Parkinson’s illness with cognitive impairment: present approaches and future instructions. Behav Sci (Basel). 2021;11(4):54.
42. Rolinski M, Fox C, Maidment I, McShane R. Cholinesterase inhibitors for dementia with Lewy our bodies, Parkinson’s illness dementia and cognitive impairment in Parkinson’s illness. Cochrane Database Syst Rev. 2012;2012(3):CD006504.
43. Wang HF, Yu JT, Tang SW, et al. Efficacy and security of cholinesterase inhibitors and memantine in cognitive impairment in Parkinson’s illness, Parkinson’s illness dementia, and dementia with Lewy our bodies: systematic evaluation with meta-analysis and trial sequential evaluation. J Neurol Neurosurg Psychiatry. 2015;86(2):135-143.
44. Pagano G, Rengo G, Pasqualetti G, et al. Cholinesterase inhibitors for Parkinson’s illness: a scientific evaluation and meta-analysis. J Neurol Neurosurg Psychiatry. 2015;86(7):767-773.
45. Meng YH, Wang PP, Track YX, Wang JH. Cholinesterase inhibitors and memantine for Parkinson’s illness dementia and Lewy physique dementia: a meta-analysis. Exp Ther Med. 2019;17(3):1611-1624.

