SPECIAL REPORT: SLEEP DISORDERS
Insomnia happens in as much as 90% of people with signs of despair, nervousness, or misery.1 Traditionally, when insomnia signs occurred within the presence of different psychological and bodily well being situations, the insomnia was considered as a secondary symptom of the comorbidity (ie, despair inflicting and sustaining insomnia).2 In lots of instances, psychiatric signs might straight trigger and preserve patterns of rumination and damaging considering all through the evening, finally resulting in the event of insomnia.1,3 Nonetheless, a considerable physique of proof now means that the connection between insomnia and psychiatric signs is extra complicated, so there may be robust rationale for focused administration of sleep issues within the presence of psychiatric signs.3-10 On this article, we offer latest proof on the bidirectional relationship between sleep and psychiatric signs to help the focused evaluation and administration of comorbid insomnia in psychological well being settings.
Cognitive conduct remedy for insomnia (CBT-I) is the really useful first-line therapy for insomnia in US and worldwide tips.11-14 Nonetheless, CBT-I is accessed by only a few people with insomnia dysfunction,15 together with by purchasers in psychological well being settings. One of many predominant obstacles is a scarcity of clinicians skilled in insomnia evaluation or the supply of CBT-I.16
Current Proof
What’s insomnia?
Insomnia diagnostic standards consists of self-reported difficulties falling asleep and/or sustaining sleep on at the very least 3 nights per week, with related daytime purposeful/feeling impairment, within the context of enough time in mattress and alternative for sleep.17 Insomnia can additional be labeled as a short-term situation if persisting for lower than 3 months (which happens in roughly 30% to 40% of adults at any given time) or a continual situation if persisting for at the very least 3 months (which happens in roughly 15% of adults at any given time).17 At a dysfunction stage, insomnia and despair additionally share vital overlap; sleep disturbance is listed amongst diagnostic standards for main depressive dysfunction, and lowered temper is listed amongst diagnostic standards for insomnia dysfunction.17,18
Is it secondary insomnia or comorbid insomnia?
Quick-term sleep disturbance may result from many various psychological, bodily, circadian, environmental, and life-style elements.19 Nonetheless, insomnia signs can rapidly develop purposeful independence from the preliminary causes and turn out to be a self-maintaining continual situation.20 For instance, psychiatric signs might trigger preliminary sleep disturbances; nevertheless, people might begin spending extra time in mattress with the purpose of buying extra sleep, leading to extra time awake in mattress experiencing frustration or fear about sleep loss, and a realized relationship can develop whereby the mattress or bed room turns into an automated stimulus for alertness and wakefulness as a substitute of sleep.21 In people presenting with insomnia and psychiatric signs, it’s not often attainable to find out whether or not the insomnia is a secondary symptom of the psychological well being situation, a self-maintaining comorbid dysfunction, or strengthened by a mixture of psychiatric and self-maintaining elements.3 For that reason, diagnostic schema have moved away from the time period secondary insomnia and as a substitute use the time period insomnia dysfunction, which captures insomnia presenting as an impartial or comorbid situation, emphasizing the significance of focused evaluation and administration of insomnia as a self-maintaining and treatable situation, no matter any comorbidity.17
Which comes first, insomnia or psychiatric signs?
Epidemiological research have discovered that despair can predict the event of insomnia and that insomnia signs can predict the event of despair.3 For instance, a scientific evaluation and meta-analysis of 21 research by Baglioni et al discovered that insomnia was related to a considerably elevated threat of creating despair (OR, 2.6; 95% CI, 2.0-3.4).4 In 2019, Hertenstein et al additionally reported in a scientific evaluation and meta-analysis that insomnia is related to elevated dangers of creating despair (OR, 2.8; 95% CI, 1.6-5.2), nervousness (OR, 3.2; 95% CI, 1.5-6.9), alcohol abuse (OR, 1.4; 95% CI, 1.1-1.7), and psychosis (OR, 1.3; 95% CI, 1.3-1.6).22 These research spotlight the potential bidirectional relationship between sleep and psychiatric signs and the significance of sleep disturbance within the prodromal phases or as a causal contributor to psychological well being decline.
Can insomnia be handled within the presence of psychiatric signs?
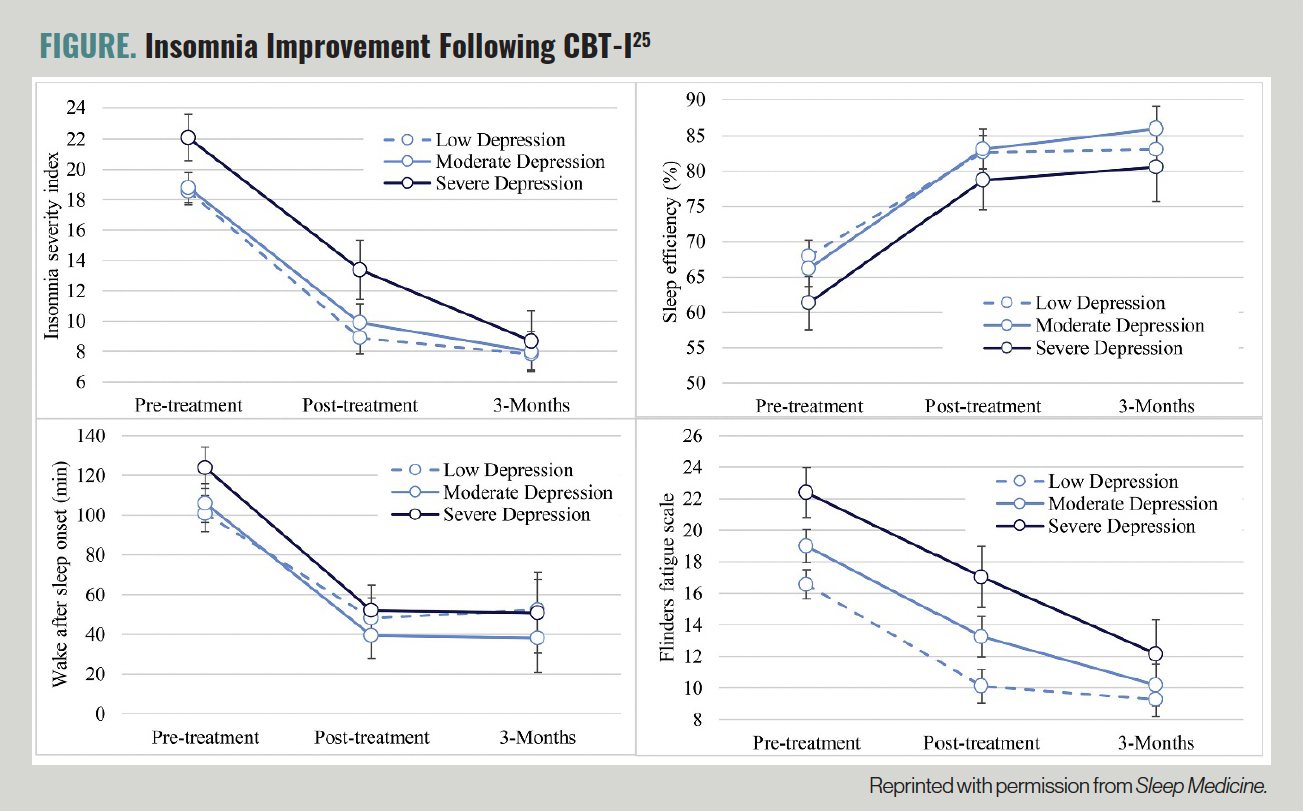
CBT-I is commonly delivered over 4 to eight periods that purpose to establish and step by step deal with the psychobehavioral elements that trigger and preserve insomnia and any realized relationship between the bed room surroundings and an automated state of alertness and wakefulness.12 In contrast to sedative-hypnotic medicines that quickly goal the floor signs of insomnia,23 CBT-I goals to focus on the underlying elements that preserve insomnia and is related to reasonable to massive enhancements in insomnia signs which might be sustained over time.24 We lately investigated in 455 people presenting to an outpatient CBT-I program whether or not these with signs of despair, nervousness, or stress skilled much less profit from CBT-I vs these with out psychiatric signs.25 If insomnia is a secondary symptom of psychiatric signs, it might be anticipated that these with extra extreme psychiatric signs would expertise much less profit from CBT-I. Nonetheless, we discovered that people with delicate, reasonable, and extreme ranges of despair, nervousness, and stress skilled related ranges of insomnia enchancment following CBT-I (Determine).25 These insomnia enhancements had been additionally maintained 3 months submit therapy.25
FIGURE. Insomnia Enchancment Following CBT-I25
Does insomnia therapy enhance psychiatric signs?
Enhancing sleep has a optimistic downstream impact on psychological well being. Equally, treating insomnia with CBT-I can enhance comorbid psychiatric signs.3 For instance, meta-analyses have reported reasonable to massive results of insomnia therapy on bettering despair7,8 and nervousness signs in individuals with insomnia.26 Within the aforementioned examine of 455 people with insomnia handled with CBT-I, we additionally noticed reasonable to massive and sustained enhancements in signs of despair, nervousness, and stress after insomnia was handled with CBT-I.25
Does insomnia therapy forestall psychiatric signs?
As talked about beforehand, insomnia can improve an individual’s threat of creating despair4,22 and treating insomnia with CBT-I can enhance insomnia and psychiatric signs.7,8,26 Subsequently, it could be attainable to establish and deal with insomnia to forestall the event or development of psychiatric signs. That’s, early therapy of insomnia might forestall despair. A latest systematic evaluation by Boland et al discovered 6 analysis research that investigated the impact of CBT-I on charges of incident main depressive dysfunction.27 4 research discovered that CBT-I used to be related to a lowered incidence of main depressive dysfunction, and a couple of failed to verify these ends in main analyses (though secondary analyses had been according to a preventive impact of CBT-I on despair signs28).27 Though extra analysis is required, these are promising findings that point out that early identification and therapy of sleep issues could also be one technique to forestall the onset and development of psychiatric signs.
Enhancing the Administration of Insomnia in Australia
Regardless of the established effectiveness of CBT-I and the potential to capitalize on the antidepressant results of CBT-I in psychological well being settings, only a few people with insomnia obtain CBT-I.15 For instance, in a latest evaluation of greater than 5 million veterans within the Veterans Well being Administration, CBT-I used to be offered to solely 0.2% of sufferers.29 In Australia, roughly 90% of main care sufferers with insomnia are managed with sedative-hypnotic medicines and just one% are referred for CBT-I.30,31 One of many predominant obstacles is a really restricted variety of clinicians skilled in CBT-I supply. In a 2020-2021 audit of the variety of psychologists in Australia specializing within the administration of insomnia, the Australasian Sleep Affiliation recognized solely 65 sleep psychologists nationally.32
To extend the supply of clinicians skilled to ship CBT-I, the Australasian Sleep Affiliation and Australian Psychological Society have collaborated on an insomnia training and implementation marketing campaign during the last 6 years. The training marketing campaign has resulted in on-line and print articles on insomnia administration in psychological well being settings,33 webinars on insomnia and CBT-I, the event and promotion of an interactive 6-hour CBT-I training module and downloadable manualized CBT-I program,34 a sequence of seven webinars on insomnia administration in various and comorbid populations, convention attendance for psychological well being and life-style drugs specialists, and the event of a brand new CBT-I supplier listing itemizing Australian and New Zealand clinicians who’ve efficiently accomplished coaching in CBT-I.35 Extra insomnia and CBT-I training can be required for psychiatrists, psychological well being nurses, and the broader psychological well being workforce. Nonetheless, our flagship interactive CBT-I training program will be accessed by any psychological well being practitioners in Australia and internationally.34
By mid-2026, this training marketing campaign is predicted to succeed in greater than 3000 psychologists,36 representing a considerable improve from the 65 acknowledged sleep psychologists in 2020.32 These training and implementation actions have been funded by a 2021 Australian authorities grant program awarded to the Australasian Sleep Affiliation, and they’re solely attainable due to a optimistic and sustained collaboration between the Australasian Sleep Affiliation and Australian Psychological Society and the fervour and dedication of many voluntary members and workers. We hope that these training actions will step by step enhance the administration of sleep issues in Australian psychological well being settings and that our work might inform related implementation actions in different areas.
Concluding Ideas
Insomnia and psychiatric signs regularly co-occur in psychological well being settings. Though insomnia has traditionally been considered as a secondary symptom of psychiatric situations, there may be now a considerable physique of proof indicating that sleep and psychological well being are bidirectionally associated. Nonpharmacological therapy of insomnia is efficient within the presence of psychiatric signs; reduces the severity of preexisting despair, nervousness, and stress; and should scale back an individual’s threat of creating psychiatric signs sooner or later. Subsequently, psychological well being practitioners might take into account the administration of insomnia and sleep issues alongside therapy of psychiatric signs.
To extend affected person entry to CBT-I, it’s important to work collaboratively throughout the sleep and psychological well being sector to help extra psychological well being practitioners accessing CBT-I coaching, assets, and help. Our joint training program has step by step improved recognition of insomnia in Australian psychological settings. We hope that it will enhance CBT-I entry within the better neighborhood and will probably be helpful in informing related worldwide implementation and teaching programs.
Dr Sweetman is a senior program supervisor on the Australasian Sleep Affiliation and has tutorial standing at Flinders College, Bond College, and the College of Western Australia. Ms Papadopoulos is head of training, coaching, and assessments on the Australian Psychological Society. Ms Balzer is chief govt officer on the Australasian Sleep Affiliation.
Disclosures: Dr Sweetman is a workers member of the Australasian Sleep Affiliation, experiences unrelated analysis tools and/or funding help from the Australian Authorities Division of Well being and Aged Care, Nationwide Well being and Medical Analysis Council, Medical Analysis Future Fund, Flinders College, Flinders Basis, Hospital Analysis Basis Group, Huge Well being, Philips Respironics, Compumedics Restricted, Western Australian Suicide Prevention and Resilience Analysis Centre, American Academy of Sleep Drugs, and Panthera; unrelated commissioned/consultancy work for Australian Physician Group, Sleep Overview journal, Re-Time Australia, Air Liquide, and Resmed; and unrelated honorarium from the American Academy of Dental Sleep Drugs, Taiwan Society of Sleep Drugs, TMJ Remedy Centres, Cerebra, and the Australian and New Zealand Academy of Orofacial Ache, and is codeveloper of a digital CBT for insomnia program (Bedtime Window).
References
1. Staner L. Comorbidity of insomnia and despair. Sleep Med Rev. 2010;14(1):35-46.
2. Lichstein KL. Secondary insomnia: a fable dismissed. Sleep Med Rev. 2006;10(1):3-5.
3. Sweetman A, Lack L, Van Ryswyk E, et al. Co-occurring despair and insomnia in Australian main care: latest scientific proof. Med J Aust. 2021;215(5):230-236.
4. Baglioni C, Battagliese G, Feige B, et al. Insomnia as a predictor of despair: a meta-analytic analysis of longitudinal epidemiological research. J Have an effect on Disord. 2011;135(1-3):10-19.
5. Blom Okay, Jernelöv S, Kraepelien M, et al. Web therapy addressing both insomnia or despair, for sufferers with each diagnoses: a randomized trial. Sleep. 2015;38(2):267-277.
6. Cheng P, Kalmbach DA, Tallent G, et al. Despair prevention by way of digital cognitive behavioral remedy for insomnia: a randomized managed trial. Sleep. 2019;42(10):zsz150.
7. Cunningham JEA, Shapiro CM. Cognitive behavioural remedy for insomnia (CBT-I) to deal with despair: a scientific evaluation. J Psychosom Res. 2018;106:1-12.
8. Gebara MA, Siripong N, DiNapoli EA, et al. Impact of insomnia remedies on despair: a scientific evaluation and meta‐evaluation. Depress Nervousness. 2018;35(8):717-731.
9. Li L, Wu C, Gan Y, et al. Insomnia and the danger of despair: a meta-analysis of potential cohort research. BMC Psychiatry. 2016;16(1):375.
10. Riemann D, Krone LB, Wulff Okay, Nissen C. Sleep, insomnia, and despair. Neuropsychopharmacology. 2020;45(1):74-89.
11. Qaseem A, Kansagara D, Forciea MA, et al. Administration of continual insomnia dysfunction in adults: a scientific apply guideline from the American School of Physicians. Ann Intern Med. 2016;165(2):125-133.
12. Edinger JD, Arnedt JT, Bertisch SM, et al. Behavioral and psychological remedies for continual insomnia dysfunction in adults: an American Academy of Sleep Drugs systematic evaluation, meta-analysis, and GRADE evaluation. J Clin Sleep Med. 2021;17(2):263-298.
13. Wilson S, Anderson Okay, Baldwin D, et al. British Affiliation for Psychopharmacology consensus assertion on evidence-based therapy of insomnia, parasomnias and circadian rhythm problems: an replace. J Psychopharmacol. 2019;33(8):923-947.
14. Ree M, Junge M, Cunnington D. Australasian Sleep Affiliation place assertion concerning the usage of psychological/behavioral remedies within the administration of insomnia in adults. Sleep Med. 2017;36(suppl 1):S43-S47.
15. Sweetman A, McEvoy RD, Frommer MS, et al. Selling sustained entry to cognitive behavioral remedy for insomnia in Australia: a system-level implementation program. J Clin Sleep Med. 2025;21(2):325-335.
16. Meaklim H, Rehm IC, Monfries M, et al. Get up psychology! postgraduate psychology college students want extra sleep and insomnia training. Aust Psychol. 2021:56(6):485-498.
17. Worldwide Classification of Sleep Problems. third ed. American Academy of Sleep Drugs; 2014.
18. American Psychiatric Affiliation. Diagnostic and Statistical Handbook of Psychological Problems. fifth ed, textual content revision. American Psychiatric Affiliation; 2022.
19. Bastien CH, Vallières A, Morin CM. Precipitating elements of insomnia. Behav Sleep Med. 2004;2(1):50-62.
20. Spielman AJ, Caruso LS, Glovinsky PB. A behavioral perspective on insomnia therapy. Psychiatr Clin North Am. 1987;10(4):541-553.
21. Spielman AJ, Saskin P, Thorpy MJ. Remedy of continual insomnia by restriction of time in mattress. Sleep. 1987;10(1):45-56.
22. Hertenstein E, Feige B, Gmeiner T, et al. Insomnia as a predictor of psychological problems: a scientific evaluation and meta-analysis. Sleep Med Rev. 2019;43:96-105.
23. Sweetman A, Putland S, Lack L, et al. The impact of cognitive behavioural remedy for insomnia on sedative-hypnotic use: a story evaluation. Sleep Med Rev. 2020;56:101404.
24. van der Zweerde T, Bisdounis L, Kyle SD, et al. Cognitive behavioral remedy for insomnia: a meta-analysis of long-term results in managed research. Sleep Med Rev. 2019;48:101208.
25. Sweetman A, Lovato N, Micic G, et al. Do signs of despair, nervousness or stress impair the effectiveness of cognitive behavioral remedy for insomnia? a chart-review of 455 sufferers with continual insomnia. Sleep Med. 2020;75:401-410.
26. Belleville G, Cousineau H, Levrier Okay, St-Pierre-Delorme MÈ. Meta-analytic evaluation of the impression of cognitive-behavior remedy for insomnia on concomitant nervousness. Clin Psychol Rev. 2011;31(4):638-652.
27. Boland EM, Goldschmied JR, Gehrman PR. Does insomnia therapy forestall despair? Sleep. 2023;46(6):zsad104.
28. Christensen H, Batterham PJ, Gosling JA, et al. Effectiveness of an internet insomnia program (SHUTi) for prevention of depressive episodes (the GoodNight Examine): a randomised managed trial. Lancet Psychiatry. 2016;3(4):333-341.
29. Pfeiffer PN, Ganoczy D, Zivin Okay, et al. Guideline-concordant use of cognitive behavioral remedy for insomnia within the Veterans Well being Administration. Sleep Well being. 2023;9(6):893-896.
30. Miller CB, Valenti L, Harrison CM, et al. Time tendencies within the household doctor administration of insomnia: the Australian expertise (2000-2015). J Clin Sleep Med. 2017;13(6):785-790.
31. Haycock J, Lack L, Hoon E, et al. O048 assist in search of behaviours of Australian adults with insomnia in a neighborhood pattern. Sleep Adv. 2022;3(suppl 1):A20.
32. Sweetman A, McEvoy RD, Frommer MS, et al. Selling sustained entry to cognitive behavioral remedy for insomnia in Australia: a system-level implementation program. J Clin Sleep Med. 2025;21(2):325-335.
33. Winter S, Meaklim H, Kennedy G, et al. Sleep issues in psychological apply. InPsych. 2022;44.
34. CBT for Insomnia (CBTi) licensed expertise course. Australian Psychological Society. Accessed April 17, 2025. https://psychology.org.au/occasion/24371
35. Sleep central: CBTi supplier listing. Australasian Sleep Affiliation. Accessed April 17, 2025. https://sleep.org.au/Central/Contents/Clinicians-CBTi.aspx
36. Over 22,000 main care workers offered sleep training by way of ASA grants. Australasian Sleep Affiliation. February 5, 2025. Accessed April 17, 2025. https://www.sleep.org.au/Public/Information/F-ASA-news/Feb/ASA-grants.aspx

