SPECIAL REPORT: SLEEP DISORDERS
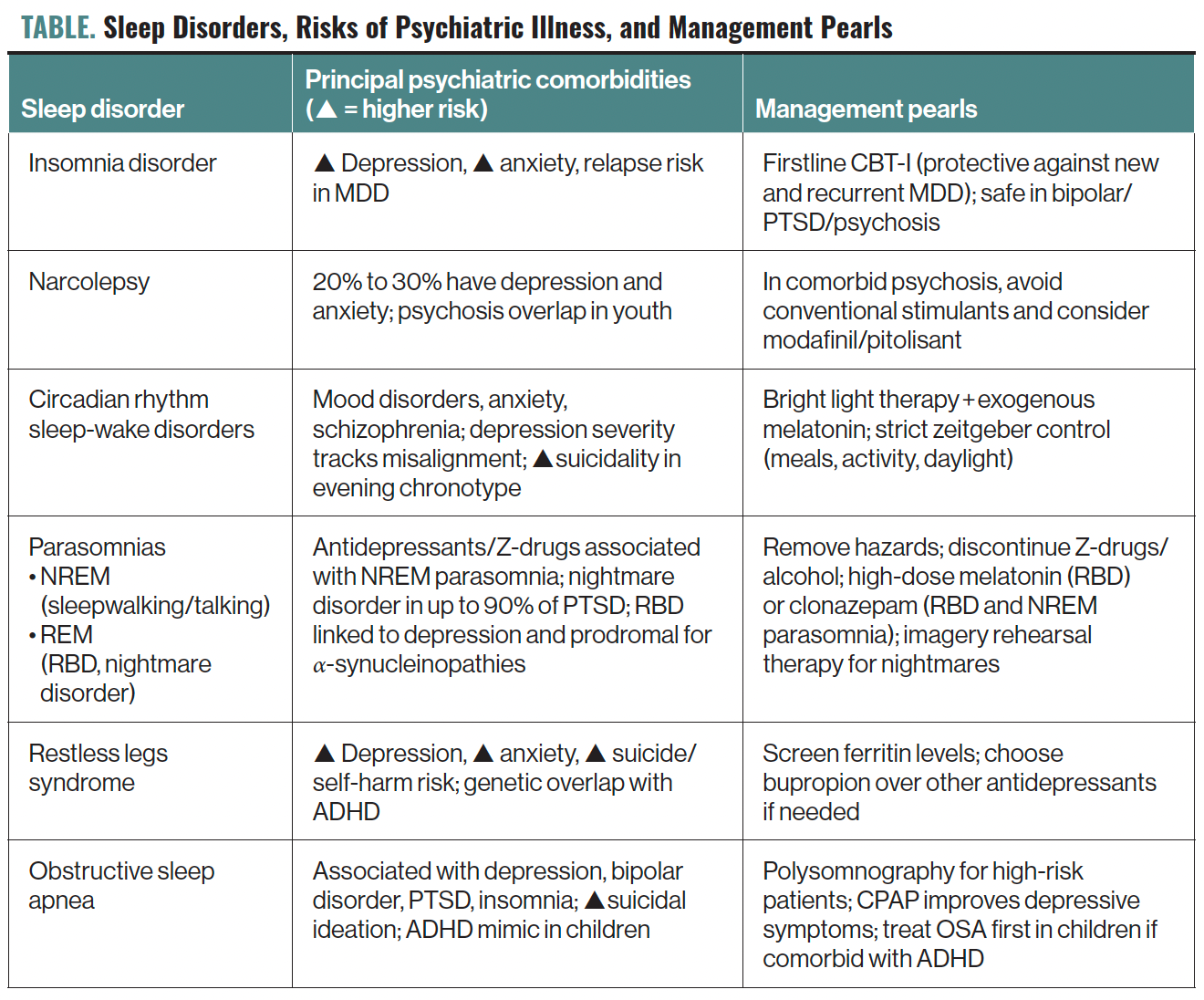
Sleep issues embody a spread of situations characterised by disturbances in sleep patterns and embody insomnia, hypersomnia, circadian rhythm disturbances, parasomnias, sleep-related motion issues, and sleep-related respiration issues. Psychiatric signs typically coexist with sleep issues, creating diagnostic and therapeutic complexities. Understanding these psychiatric manifestations is essential for clinicians to handle each sleep issues and psychiatric situations successfully (see the Desk for sleep issues, their associations with psychiatric diseases, and administration pearls). Sleep disturbances can exacerbate psychiatric signs, and conversely, psychiatric situations typically worsen sleep issues, demonstrating a reciprocal relationship that warrants detailed exploration.
TABLE. Sleep Issues, Dangers of Psychiatric Sickness, and Administration Pearls
Insomnia Dysfunction
Continual insomnia dysfunction is characterised by difficulties falling or staying asleep at the least 3 occasions per week for at the least 3 months, resulting in useful impairment. Sufferers with insomnia dysfunction are 3 occasions extra prone to develop nervousness and melancholy.1 Residual sleep disturbance in main depressive dysfunction (MDD) is related to attenuated remedy impact and depressive relapse.2 The primary-line remedy, cognitive habits remedy for insomnia (CBT-I), has demonstrated a protecting impact towards incident and recurrent MDD.2 CBT-I and tailored codecs have sturdy proof for safely treating insomnia in comorbid bipolar dysfunction, nervousness, posttraumatic stress dysfunction (PTSD), and psychosis.3 Some sufferers with insomnia could obtain on-label hypnotics reminiscent of Z-drugs and twin orexin receptor antagonists. For these with comorbid melancholy, sedating antidepressants reminiscent of trazodone or mirtazapine could deal with each situations.
Mechanistically, insomnia contributes to psychiatric signs by inappropriate sympathetic nervous activation, altered hypothalamic-pituitary-adrenal axis perform, and larger systemic inflammatory response.4 Neuroimaging research reveal that sufferers with power insomnia show variations within the anterior cingulate cortex, thalamus, insula, precuneus, and center frontal gyrus.4
Central Issues of Hypersomnolence
Probably the most placing of the hypersomnolence issues is narcolepsy. The narcolepsy issues share signs of extreme daytime sleepiness, sleep paralysis, sleep-related hallucinations, and disturbed nighttime sleep, however they’re differentiated by the presence of cataplexy and hypocretin deficiency in narcolepsy kind 1. One other dysfunction is idiopathic hypersomnia, through which sufferers show the discovering of brief sleep latency on a number of sleep latency testing however the absence of irregular sleep-onset REM durations. They could display a routine sleep length of greater than 660 minutes per 24 hours. Hypersomnolence itself could also be seen in sufferers with main or bipolar melancholy. Despair and nervousness are present in 20% to 30% of people with narcolepsy.5 There’s larger overlap of narcolepsy with psychotic issues in people youthful than 16 years, which can implicate a attainable shared neurodegenerative mechanism.6 Hypocretin—a neurotransmitter that promotes wakefulness and suppresses REM sleep—is poor in narcolepsy, which might be the results of an autoimmune response, head harm, tumor, or environmental results.5 Care must be taken in prognosis to distinguish the sleep-related hallucinations in narcolepsy from these in major psychosis. Administration of narcolepsy comorbid with schizophrenia might be significantly difficult, as standard stimulants reminiscent of methylphenidates and amphetamines could precipitate or exacerbate optimistic psychotic signs.6 There have been case stories of psychosis secondary to sodium oxybate remedy.6 Modafinil and pitolisant have been utilized in such overlap circumstances to keep away from exacerbation of psychosis.6 Sooner or later, hypocretin agonists could maintain promise to buttress alertness whereas avoiding psychosis exacerbation mechanistically.
Circadian Rhythm Issues
The circadian rhythm regulates a number of physiological features, together with alertness, hormone secretion, temperature regulation, and neurotransmitters essential in psychiatric issues. Misalignment of the circadian rhythm with the exterior light-dark cycle can result in functionally impairing circadian rhythm issues. These issues are widespread in temper and nervousness issues and schizophrenia, contributing to symptom exacerbation and diminished remedy efficacy.7,8 Exacerbation of psychiatric signs could partially be attributable to extra publicity to synthetic gentle, shift work, and journey between time zones. Circadian rhythm disturbances influence psychiatric well being by disrupting melatonin secretion, cortisol rhythms, and neurotransmitter cycles.7 Particular polymorphisms of clock genes have been related to seasonal melancholy, MDD, and delayed sleep-wake part dysfunction (DSWPD).7 The severity of MDD is carefully correlated with the extent of misalignment.7 Of word, a night chronotype (a bent for late sleep and wake occasions) is a robust threat issue for melancholy with larger severity of episodes and better threat for suicidality.7 A night chronotype is related to larger severity of depressive signs and fewer manic episodes in bipolar dysfunction. Circadian mismatch in bipolar dysfunction seems to be bidirectional in affiliation, and DSWPD is the most typical comorbid circadian rhythm dysfunction.7 DSWPD is characterised by a circadian rhythm that’s far delayed in contrast with norms. The imposition of socially acceptable sleep and wake occasions results in insomnia.9 It disproportionately impacts adolescents and younger adults and is related to a excessive fee of melancholy. Remedy by vibrant gentle and melatonin could normalize sleep and scale back melancholy.9 In Alzheimer illness dementia, sufferers could not exhibit any constant sample of sleep. Generally seen within the dysfunction are day-night reversals, fragmented nighttime sleep, and exorbitant quantities of daytime sleep.10 This recurrent sample of sleep disruption is pathognomonic for irregular sleep-wake kind circadian rhythm dysfunction. In schizophrenia, quite a lot of sleep-wake adjustments have been famous, together with each delayed sleep chronotypes and irregular sleep-wake patterns.8 The position of environmental cues, together with publicity to pure daylight, common meal timing, and constant exercise schedules, highlights the need of behavioral interventions alongside medical therapies to handle circadian-related psychiatric signs successfully.
Parasomnias
Parasomnias, divided into non-REM (NREM) parasomnias reminiscent of sleep speaking/sleepwalking and sleep terrors, and REM parasomnias, reminiscent of nightmare dysfunction and REM sleep habits dysfunction (RBD), often co-occur in psychiatric populations. NREM parasomnias, characterised by an incomplete dissociation between slow-wave sleep and wakefulness, could result in advanced sleep behaviors however with impaired recall. They have a tendency to happen in the course of the first third of the night time, when slow-wave sleep predominates. They’re seen in larger prevalence in psychiatric populations, significantly those that use antidepressants and Z-drugs.11 Of word, zolpidem has been implicated in precipitating sleepwalking and sleep-related consuming dysfunction. Nightmare dysfunction, which is current in as much as 90% of people with PTSD, is related to larger nervousness and depressive signs and elevated suicidality.11 RBD, characterised by dream enactment behaviors that may embody each actions and speech because of lack of muscle atonia in REM sleep and might be related to harm to the affected person or mattress associate, is strongly linked to a-synuclein illness, reminiscent of Parkinson illness, and is related to melancholy.11 It typically happens over the last third or half of the night time, when REM sleep predominates. These with RBD could recall their actions as congruent with dream content material if awoken.
Scientific administration of parasomnias embody behavioral interventions reminiscent of avoidance of offending brokers together with alcohol and Z-drugs in NREM circumstances, putting boundaries strategically with mushy padding for the ground, and eradicating weapons and breakable objects from the bed room to make sure security. Pharmacological therapies could embody high-dose melatonin for RBD and clonazepam in each RBD and NREM parasomnias after different sleep issues have been dominated out or handled.12 Imagery rehearsal remedy, whereby sufferers rewrite the endings of their recurrent nightmares for the higher, is efficient in decreasing nightmares in comorbid melancholy, nervousness, and PTSD, and it demonstrates early optimistic proof in borderline character dysfunction.13
Stressed Legs Syndrome
Stressed legs syndrome (RLS) is characterised by uncomfortable sensations within the extremities that normally happen within the hours previous bedtime, resulting in an urge to maneuver that’s worse with inactivity and improves with motion. This may trigger issue with sleep initiation and upkeep, resulting in sleep deprivation. It’s related to being pregnant, end-stage renal illness, neuropathy, and disturbances in iron and dopamine metabolism. It seems to be considerably related to psychiatric pathology. Up to date meta-analytic proof reveals that sufferers with RLS have a major enhance in melancholy and nervousness in contrast with controls.14 Mendelian randomization means that attention-deficit/hyperactivity dysfunction (ADHD) is an impartial genetic threat issue for RLS, implicating shared dopaminergic and iron metabolism pathways and suggesting a larger relationship than mere symptomatic overlap.15 Giant longitudinal cohorts display that RLS confers a 2 to 3-fold enhance in suicide or self-harm threat even after adjustment for way of life elements, different sleep issues, melancholy, and different power illnesses.16 Remedy concerns in circumstances of comorbid melancholy and nervousness give attention to remedy choice. Many antidepressants could precipitate or exacerbate RLS, with bupropion being the exception.17 Remedy by dopamine agonists isn’t really helpful due to the augmentation dangers (signs worsening and requiring larger remedy doses to regulate) over time. Gabapentinoids at the moment are thought of the first-line pharmacotherapy.
Obstructive Sleep Apnea
Obstructive sleep apnea (OSA) describes recurrent higher airway collapse, normally related to weight problems and higher airway anatomical challenges. Consequently, sufferers expertise hypoxic occasions and repeated disruptions from sleep all through the night time. This may increasingly mediate its affiliation with melancholy, bipolar dysfunction, PTSD, insomnia, extreme daytime sleepiness, and cognitive impairment.18
OSA will increase the danger of hypertension, stroke, myocardial infarction, and motorized vehicle accidents. Untreated OSA considerably will increase the danger of suicidal ideation even after controlling for melancholy and substance use.18 Within the pediatric inhabitants, there’s a well-established overlap of symptomatology between OSA and ADHD, the place remedy of the previous could spare sufferers from stimulant remedy.19
Steady optimistic airway strain remedy stays the cornerstone of remedy and has been demonstrated to result in enchancment in melancholy in comorbid circumstances, whereas proof for mandibular advance units seems unfavourable for an impact on melancholy in a meta-analysis.20
Diagnostic and Scientific Implications
Correct identification of sleep issues alongside psychiatric issues is crucial. Clinicians ought to refer sufferers for polysomnography or house sleep testing when acceptable (eg, loud night breathing, excessive physique mass index, treatment-resistant hypertension, advanced nighttime behaviors, RLS signs, or extreme daytime sleepiness). Early recognition and focused remedy of sleep issues could enhance psychiatric outcomes, highlighting the necessity for built-in sleep-psychiatric care. Clinicians should additionally take into account remedy results, substance use, and comorbid medical situations that additional complicate the relationships between psychiatric issues. Collaborative care fashions integrating psychiatrists, sleep specialists, and first care suppliers are wanted to optimize affected person outcomes.
Concluding Ideas
Sleep issues considerably contribute to psychiatric symptomatology, creating advanced diagnostic and therapeutic challenges. Understanding the bidirectional relationship between sleep and psychiatric well being is important for efficient medical administration. Enhanced consciousness, exact prognosis, and built-in therapeutic approaches can considerably enhance each psychiatric and sleep outcomes. Future analysis ought to additional elucidate underlying mechanisms, enhance diagnostic accuracy, and optimize built-in remedy methods.
Dr Mak is a psychiatrist and sleep drugs specialist on the Centre for Habit and Psychological Well being and an assistant professor within the Division of Psychiatry on the College of Toronto. Dr Choi is a resident doctor within the Division of Psychiatry on the College of Toronto. Mr Siddiqui is a scholar at McMaster College. Dr Tomatsu is a fellow on the Middle for Circadian and Sleep Medication within the Division of Neurology, Division of Sleep Medication at Northwestern College and adjunct medical assistant professor within the Division of Psychiatry at Wake Forest College in Charlotte, North Carolina. Dr Gazzellone is a medical fellow in sleep problem drugs within the Division of Psychiatry on the College of Toronto.
References
1. Hertenstein E, Benz F, Schneider CL, Baglioni C. Insomnia—a threat issue for psychological issues. J Sleep Res. 2023;32(6):e13930.
2. Mak MSB, Gebara MA, Lenze EJ, et al. Poor sleep is widespread in treatment-resistant late-life melancholy and related to poorer antidepressant response: findings from the OPTIMUM medical trial. Am J Geriatr Psychiatry. 2025;33(1):63-72.
3. Jansson-Fröjmark M, Norell-Clarke A. Cognitive behavioural remedy for insomnia in psychiatric issues. Curr Sleep Med Rep. 2016;2(4):233-240.
4. Aquino G, Benz F, Dressle RJ, et al. In direction of the neurobiology of insomnia: a scientific assessment of neuroimaging research. Sleep Med Rev. 2024;73:101878.
5. Bassetti CLA, Adamantidis A, Burdakov D, et al. Narcolepsy—medical spectrum, aetiopathophysiology, prognosis, and remedy. Nat Rev Neurol. 2019;15(9):519-539.
6. Hanin C, Arnulf I, Maranci JB, et al. Narcolepsy and psychosis: a scientific assessment. Acta Psychiatr Scand. 2021;144(1):28-41.
7. Dollish HK, Tsyglakova M, McClung CA. Circadian rhythms and temper issues: time to see the sunshine. Neuron. 2024;112(1):25-40.
8. Wulff Okay, Dijk DJ, Middleton B, et al. Sleep and circadian rhythm disruption in schizophrenia. Br J Psychiatry. 2012;200(4):308-316.
9. Rahman SA, Kayumov L, Shapiro CM. Antidepressant motion of melatonin within the remedy of delayed sleep part syndrome. Sleep Med. 2010;11(2):131-136.
10. Zhang Y, Ren R, Yang L, et al. Sleep in Alzheimer’s illness: a scientific assessment and meta-analysis of polysomnographic findings. Transl Psychiatry. 2022;12(1):136.
11. Waters F, Moretto U, Dang-Vu TT. Psychiatric sickness and parasomnias: a scientific assessment. Curr Psychiatry Rep. 2017;19(7):37.
12. Hurwitz TD, Howell M, Khawaja IS. Parasomnias: a assessment for psychiatrists. FOCUS J Lifelong Study Psychiatry. 2014;12(1):16-30.
13. Sayk C, Koch N, Stierand J, et al. Imagery rehearsal remedy for the remedy of nightmares in people with borderline character dysfunction—a pilot research. J Psychiatr Res. 2025;182:34-41.
14. An T, Solar H, Yuan L, et al. Associations of tension and melancholy with stressed leg syndrome: a scientific assessment and meta-analysis. Entrance Neurol. 2024;15:1366839.
15. Xiao G, Shi H, Lan Q, et al. Affiliation amongst attention-deficit hyperactivity dysfunction, stressed legs syndrome, and peripheral iron standing: a two-sample Mendelian randomization research. Entrance Psychiatry. 2024;15:1310259.
16. Zhuang S, Na M, Winkelman JW, et al. Affiliation of stressed legs syndrome with threat of suicide and self-harm. JAMA Netw Open. 2019;2(8):e199966.
17. Silber MH, Buchfuhrer MJ, Earley CJ, et al. The administration of stressed legs syndrome: an up to date algorithm. Mayo Clin Proc. 2021;96(7):1921-1937.
18. Benca RM, Krystal A, Chepke C, Doghramji Okay. Recognition and administration of obstructive sleep apnea in psychiatric observe. J Clin Psychiatry. 2023;84(2):22r14521.
19. Urbano GL, Tablizo BJ, Moufarrej Y, et al. The hyperlink between pediatric obstructive sleep apnea (OSA) and a spotlight deficit hyperactivity dysfunction (ADHD). Kids (Basel). 2021;8(9):824.
20. Fu W, Li L, Zhang S, et al. Results of CPAP and mandibular development units on depressive signs in sufferers with obstructive sleep apnea: a meta-analysis of randomized managed trials. Sleep Breath. 2023;27(6):2123-2137.

